Helicobacter pylori
2008/9 Schools Wikipedia Selection. Related subjects: Health and medicine; Organisms
| Helicobacter pylori | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 |
||||||||||||||
| Scientific classification | ||||||||||||||
|
||||||||||||||
| Binomial name | ||||||||||||||
| Helicobacter pylori ((Marshall et al. 1985) Goodwin et al. 1989) ICD-9 code: 041.86 |
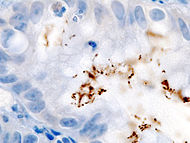
Helicobacter pylori (pronounced /ˌhɛlɪkəˈbæktɚ paɪˈlɔəraɪ} or British {pronEng/) is a gram-negative, microaerophilic bacterium that infects various areas of the stomach and duodenum. Many cases of peptic ulcers, gastritis, duodenitis, and cancers are caused by H. pylori infections. However, many who are infected do not show any symptoms of disease. H. pylori's helical shape (from which the genus name is derived) is thought to have evolved to penetrate and favour its motility in the mucus gel layer.
History
In 1875, German scientists found helical shaped bacteria in the lining of the human stomach. The bacteria could not be grown in culture and the results were eventually forgotten. In 1893, the Italian researcher Giulio Bizzozero described helical shaped bacteria living in the acidic environment of the stomach of dogs. Professor Walery Jaworski of the Jagiellonian University in Kraków investigated sediments of gastric washings obtained from humans in 1899. Among some rod-like bacteria, he also found bacteria with a characteristic helical shape, which he called Vibrio rugula. He was the first to suggest a possible role of this organism in the pathogeny of gastric diseases. This work was included in the "Handbook of Gastric Diseases", but it did not have much impact because it was written in Polish.
The bacterium was rediscovered in 1979 by Australian pathologist Robin Warren, who did further research on it with Australian physician Barry Marshall beginning in 1981; they isolated the organisms from mucosal specimens from human stomachs and were the first to successfully culture them. In their original paper, Warren and Marshall contended that most stomach ulcers and gastritis were caused by infection by this bacterium and not by stress or spicy food as had been assumed before.
The medical community was slow to recognize the role of this bacterium in stomach ulcers and gastritis, believing that no microorganism could survive for long in the acidic environment of the stomach. The community began to come around after further studies were done, including one in which Marshall drank a Petri dish of H. pylori, developed gastritis, and the bacteria were recovered from his stomach lining, thereby satisfying three out of the four of Koch's postulates. The fourth was satisfied after a second endoscopy ten days after inoculation revealed signs of gastritis and the presence of "H. pylori". Marshall was then able to treat himself using a fourteen day dual therapy with bismuth salts and metronidazole. Marshall and Warren went on to show that antibiotics are effective in the treatment of many cases of gastritis. In 1994, the National Institutes of Health (USA) published an opinion stating that most recurrent gastric ulcers were caused by H. pylori, and recommended that antibiotics be included in the treatment regimen. Evidence has been accumulating to suggest that duodenal ulcers are also associated with H. pylori infection. In 2005, Warren and Marshall were awarded the Nobel Prize in Medicine for their work on H. pylori.
Before the appreciation of the bacterium's role, stomach ulcers were typically treated with medicines that neutralize gastric acid or decrease its production. While this worked well, the ulcers very often reappeared. At one time, bismuth subsalicylate was commonly used to treat gastritis and peptic ulcers. It was often effective, but fell out of use, since its mechanism of action was a mystery. Nowadays it is quite clear that it is due to the bismuth salt acting as an antibiotic. Today, many stomach ulcers are treated with antibiotics effective against H. pylori.
The bacterium was initially named Campylobacter pyloridis, then C. pylori (after a correction to the Latin grammar) and in 1989, after DNA sequencing and other data showed that the bacterium did not belong in the Campylobacter genus, it was placed in its own genus, Helicobacter. The name pylōri means "of the pylorus" or pyloric valve (the circular opening leading from the stomach into the duodenum), from the Greek word πυλωρός, which means gatekeeper.
While H. pylori remains the most medically important bacterial inhabitant of the human stomach, other species of the Helicobacter genus have been identified in other mammals and some birds, and some of these can infect humans. Helicobacter species have also been found to infect the livers of certain mammals and to cause liver disease.
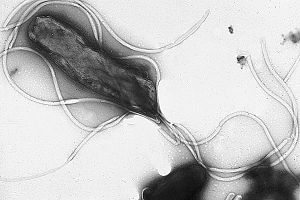
Structure
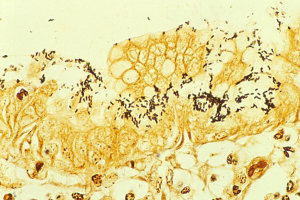
H. pylori is a helical shaped Gram-negative bacterium, about 3 micrometres long with a diameter of about 0.5 micrometre. It has 4–6 flagella. It is microaerophilic, i.e. it requires oxygen but at lower levels than those contained in the atmosphere. It contains a hydrogenase which can be used to obtain energy by oxidizing molecular hydrogen (H2) that is produced by other intestinal bacteria. It tests positive for oxidase, catalase, and urease. It is capable of forming biofilms and conversion from helical to coccoid form, both likely to favour its survival and be factors in the epidemiology of the bacterium. The coccoid form of the organism has not been cultured, but has been found in the water supply in the US. This form has also been found to be able to adhere to gastric epithelial cells in vitro.
H. pylori possesses five major outer membrane protein (OMP) families. Each OMP appears to have specific functions. All gastric and enterohepatic Helicobacter species are highly motile due to a flagella. The characteristic sheathed flagellar filaments of helicobacters are composed of two copolymerized flagellins, FlaA and FlaB. Flagellar motility is essential for Helicobacter species to colonize the gastric mucus.
Colonization
With its flagella, the bacterium moves through the stomach lumen and drills into the mucus gel layer of the stomach. It then finds ways to live in various areas of the stomach. The known areas include: inside the mucus gel layer (with a preference for the superficial area), above epithelial cells, and inside vacuoles formed by H. pylori in epithelial cells. It produces adhesins which bind to membrane-associated lipids and carbohydrates and help its adhesion to epithelial cells. An example of this is the Lewis b antigen. It produces large amounts of urease enzymes which are localized inside and outside of the bacterium. Urease metabolizes urea (which is normally secreted into the stomach) to carbon dioxide and ammonia (which neutralizes gastric acid). The survival of H. pylori in the acidic stomach is dependent on urease, and it would eventually die without it. The ammonia that is produced is toxic to the epithelial cells, and, along with the other products of H. pylori—including protease, catalase and certain phospholipases—causes damage to those cells.
Some strains of the bacterium have a particular mechanism for "injecting" the inflammatory inducing agents peptidoglycan from their own cell wall into epithelial stomach cells. (See below for "cagA pathogenicity island" in the section Genome studies of different strains) This factor may play a role in allowing certain strains to invade host tissue.
Causes of infection
H. pylori is a contagious bacterium. Many researchers think that H. pylori is transmitted orally by means of fecal matter through the ingestion of waste tainted food or water. A clean and hygienic environment can help decrease the risk of H. pylori infection.
There is experimental evidence, however, to show that Heliobacter species are not, in fact transmitted via the fecal-oral route, but rather through oral-oral contact.
Diagnosis of infection
Diagnosis of infection is usually made by checking for dyspeptic symptoms and then doing tests which can suggest H. pylori infection. One can test noninvasively for H. pylori infection with a blood antibody test, stool antigen test, or with the carbon urea breath test (in which the patient drinks 14C- or 13C-labelled urea, which the bacterium metabolizes producing labelled carbon dioxide that can be detected in the breath). However, the most reliable method for detecting H. pylori infection is a biopsy check during endoscopy with a rapid urease test, histological examination, and microbial culture. None of the test methods is completely failsafe. Even biopsy is dependent on the location of the biopsy. Blood antibody tests, for example, range from 76% to 84% sensitivity. Some drugs can affect H. pylori urease activity and give "false negatives" with the urea-based tests.
Infection may be symptomatic or asymptomatic (without perceptible ill effects). It is estimated that up to 70% of infection is asymptomatic and that about 2/3 of the world population are infected by the bacterium, making it the most widespread infection in the world. Actual infection rates vary from nation to nation - the West (Western Europe, North America, Australasia) having rates around 25% and much higher in the Third World. In the latter, it is common, probably due to poor sanitary conditions, to find infections in children. In the United States, infection is primarily in the older generations (about 50% for those over the age of 60 compared with 20% under 40 years) and the poorest.
This is largely attributed to higher hygiene standards and widespread use of antibiotics. However, antibiotic resistance is appearing in H. pylori. There are already many metronidazole resistant strains in Europe, the United States, and developing countries.
The bacteria have been isolated from feces, saliva and dental plaque of infected patients, which suggests gastro-oral or fecal-oral as possible transmission routes.
It is widely believed that in the absence of treatment, H. pylori infection—once established in its gastric niche—persists for life. In the elderly, however, it is likely infection can disappear as the stomach's mucosa becomes increasingly atrophic and inhospitable to colonization. The proportion of acute infections that persist is not known, but several studies that followed the natural history in populations have reported apparent spontaneous elimination.
Treatment of infection
In peptic ulcer patients where infection is detected, the normal procedure is eradicating H. pylori to allow the ulcer to heal. The standard first-line therapy is a one week triple therapy. The Sydney gastroenterolgist Thomas Borody invented the first triple therapy in 1987. Today, the standard triple therapy is amoxicillin, clarithromycin and a proton pump inhibitor such as omeprazole. Variations of the triple therapy have been developed over the years, such as using a different proton pump inhibitor, as with pantoprazole or rabeprazole, or using metronidazole instead of amoxicillin in those allergic to penicillin. Such a therapy has revolutionised the treatment of peptic ulcers and has made a cure to the disease possible, where previously symptom control using antacids, H2-antagonists or proton pump inhibitors alone was the only option.
A meta-analysis of randomized controlled trials suggests that supplementation with probiotics can improve eradication rates and reduce adverse events.
Unfortunately, an increasing number of infected individuals are found to harbour antibiotic-resistant bacteria. This results in initial treatment failure and requires additional rounds of antibiotic therapy or alternative strategies such as a quadruple therapy. Bismuth compounds are also effective in combination with the above drugs. For the treatment of clarithromycin-resistant strains of H. pylori the use of levofloxacin as part of the therapy has been suggested.
Some studies show that consumption of broccoli sprouts can be effective at inhibiting H. pylori growth with sulforaphane being at least one of the active agents.
Some studies show that mastic gum can destroy H. pylori in vitro, but studies done in vivo have shown it to be ineffective in short trials.
A study done on Mongolian gerbils indicates that green tea extract can suppress H. pylori growth. Another study done in South Korea suggests that an acidic polysaccharide found in green tea is significantly effective in preventing adhesion of H. pylori to human cultures of epithelial cells.
As explained below, some authors suggest that some strains of H. pylori may be protective against certain diseases of the esophagus and cardia. Therefore, a more cautious approach than complete eradication may be necessary in some cases.
Helicobacter and cancer
Two related mechanisms by which H. pylori could promote cancer are under investigation. One mechanism involves the enhanced production of free radicals near H. pylori and an increased rate of host cell mutation. The other proposed mechanism has been called a "perigenetic pathway" and involves enhancement of the transformed host cell phenotype by means of alterations in cell proteins such as adhesion proteins. It has been proposed that H. pylori induces inflammation and locally high levels of TNF-alpha and/or interleukin 6. According to the proposed perigenetic mechanism, inflammation-associated signaling molecules such as TNF-alpha can alter gastric epithelial cell adhesion and lead to the dispersion and migration of mutated epithelial cells without the need for additional mutations in tumor suppressor genes such as genes that code for cell adhesion proteins.
Acid reflux and esophageal cancer
As the incidence of gastric cancer has decreased, the incidences of gastroesophageal reflux disease and esophageal cancer have increased dramatically. In 1996, Martin J. Blaser put forward the theory that H. pylori might also have a beneficial effect: by regulating the acidity of the stomach contents, it lowers the impact of regurgitation of gastric acid into the esophagus. While some favorable evidence has been accumulated, as of 2005 the theory is not universally accepted.
Genome studies of different strains
Several strains are known, and the genomes of two have been completely sequenced. The genome of the strain "26695" consists of about 1.7 million base pairs, with some 1550 genes. The two sequenced strains show large genetic differences, with up to 6% of the nucleosides differing.
Study of the H. pylori genome is centered on attempts to understand pathogenesis, the ability of this organism to cause disease. There are 62 genes in the "pathogenesis" category of the genome database. Both sequenced strains have an approximately 40 kb long Cag pathogenicity island (a common gene sequence believed responsible for pathogenesis) that contains over 40 genes. This pathogenicity island is usually absent from H. pylori strains isolated from humans who are carriers of H. pylori but remain asymptomatic.
The cagA gene codes for one of the major H. pylori virulence proteins. Bacterial strains that have the cagA gene are associated with an ability to cause severe ulcers. The cagA gene codes for a relatively long (1186 amino acid) protein. The CagA protein is transported into human cells where it may disrupt the normal functioning of the cytoskeleton. The cag pathogenicity island has about 30 genes part of which code for a complex type IV secretion system. After attachment of H.pylori to stomach epithelial cells, the CagA protein is injected into the epithelial cells by the type IV secretion system. The CagA protein is phosphorylated on tyrosine residues by a host cell membrane-associated tyrosine kinase. Pathogenic strains of H. pylori have been shown to activate the epidermal growth factor receptor (EGFR), a membrane protein with a tyrosine kinase domain. Activation of the EGFR by H. pylori is associated with altered signal transduction and gene expression in host epithelial cells that may contribute to pathogenesis. It has also been suggested that a c-terminal region of the CagA protein (amino acids 873–1002) can regulate host cell gene transcription independent of protein tyrosine phosphorylation. It is thought, due to cagA's low GC content relative to the rest of the helicobacter genome, that the gene was acquired by horizontal transfer from another cagA+ bacterial species.