Body mass index
2008/9 Schools Wikipedia Selection. Related subjects: Health and medicine
Based on World Health Organization data here.
The body mass index (BMI), or Quetelet index, is a statistical measure of the weight of a person scaled according to height. As such, it is useful as a population measure only, and is not appropriate for diagnosing individuals. It was invented between 1830 and 1850 by the Belgian polymath Adolphe Quetelet during the course of developing "social physics".
Body mass index is defined as the individual's body weight divided by the square of their height. The formulas universally used in medicine produce a unit of measure of kg/m2. Body mass index may be accurately calculated using either of the formulas below.
| SI units |  |
| US units |  |
 |
The factors for US units are more precisely 703.0696 and 4.882428.
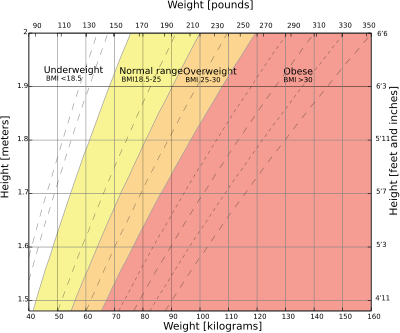
BMI can also be determined using a BMI chart, which displays BMI as a function of weight (horizontal axis) and height (vertical axis) using contour lines for different values of BMI or colors for different BMI categories.
Usage
As a measure, BMI became popular during the early 1950s and 60s as obesity started to become a discernible issue in prosperous Western societies. BMI provided a simple numeric measure of a person's "fatness" or "thinness", allowing health professionals to discuss over- and under-weight problems more objectively with their patients. However, BMI has become controversial because many people, including physicians, have come to rely on its apparent numerical authority for medical diagnosis, but that was never the BMI's purpose. It is meant to be used as a simple means of classifying sedentary (physically inactive) individuals with an average body composition. For these individuals, the current value settings are as follows: a BMI of 18.5 to 25 may indicate optimal weight; a BMI lower than 18.5 suggests the person is underweight while a number above 25 may indicate the person is overweight; a BMI below 17.5 may indicate the person has anorexia or a related disorder; a number above 30 suggests the person is obese (over 40, morbidly obese).
For a fixed body shape and body density, and given height, BMI is proportional to weight. However, for a fixed body shape and body density, and given weight, BMI is inversely proportional to the square of the height. So, if all body dimensions double, and weight scales naturally with the cube of the height, then BMI doubles instead of remaining the same. This results in taller people having a reported BMI that is uncharacteristically high compared to their actual body fat levels. This anomaly is partially offset by the fact that many taller people are not just "scaled up" short people, but tend to have narrower frames in proportion to their height. It has been suggested that instead of squaring the body height (as the BMI does) or cubing the body height (as seems natural), it would be more appropriate to use an exponent of between 2.3 to 2.7.
BMI Prime
BMI Prime, a simple modification of the BMI system, is the ratio of actual BMI to upper limit BMI (currently defined at BMI 25). As defined, BMI Prime is also the ratio of body weight to upper body weight limit, calculated at BMI 25. Since it is the ratio of two separate BMI values, BMI Prime is a dimensionless number, without associated units. Individuals with BMI Prime < 0.74 are underweight; those between 0.74 and 0.99 have optimal weight; and those at 1.00 or greater are overweight. BMI Prime is useful clinically because individuals can tell, at a glance, what percentage they deviate from their upper weight limits. For instance, a person with BMI 34 has a BMI Prime of 34/25 = 1.36, and is 36% over his or her upper mass limit. In Asian populations (see International Variation section below) BMI Prime should be calculated using an upper limit BMI of 23 in the denominator instead of 25. Nonetheless, BMI Prime allows easy comparison between populations whose upper limit BMI values differ.
Categories
A frequent use of the BMI is to assess how much an individual's body weight departs from what is normal or desirable for a person of his or her height. The weight excess or deficiency may, in part, be accounted for by body fat ( adipose tissue) although other factors such as muscularity also affect BMI significantly (see discussion below and overweight). The WHO regard a BMI of less than 18.5 as underweight and may indicate malnutrition, an eating disorder, or other health problems, while a BMI greater than 25 is considered overweight and above 30 is considered obese. These ranges of BMI values are valid only as statistical categories when applied to adults, and do not predict health.
| Category | BMI range - kg/m2 | BMI Prime | Mass of a 1.8 metres (5 ft 11 in) person with this BMI |
|---|---|---|---|
| Severely underweight | less than 16.5 | less than 0.60 | under 53.5 kilograms (8.42 st/118 lb) |
| Underweight | from 16.5 to 18.5 | from 0.6 to 0.74 | from 53.5 and 60 kilograms (8.42 and 9.45 st/118 and 132 lb) |
| Normal | from 18.5 to 25 | from 0.74 to 1.0 | from 60 and 81 kilograms (9.4 and 13 st/130 and 180 lb) |
| Overweight | from 25 to 30 | from 1.0 to 1.2 | from 81 and 97 kilograms (12.8 and 15.3 st/180 and 210 lb) |
| Obese Class I | from 30 to 35 | from 1.2 to 1.4 | from 97 and 113 kilograms (15.3 and 17.8 st/210 and 250 lb) |
| Obese Class II | from 35 to 40 | from 1.4 to 1.6 | from 113 and 130 kilograms (17.8 and 20.5 st/250 and 290 lb) |
| Obese Class III | above 40 | above 1.6 | above 130 kilograms (20 st/290 lb) |
BMI Categories within the healthy range.
Low 18.5-19.8
Med-Lo 19.9-21.1
Medium 21.2-22.4
Med-Hi 22.5-23.7
High 23.8-25.0
The U.S. National Health and Nutrition Examination Survey of 1994 indicates that 59% of American men and 49% of women have BMIs over 25. Extreme obesity — a BMI of 40 or more — was found in 2% of the men and 4% of the women. The newest survey in 2007 indicates an continuation of the increase in BMI, 63% of Americans are overweight, with 26% now in the obese category. There are differing opinions on the threshold for being underweight in females, doctors quote anything from 18.5 to 20 as being the lowest weight, the most frequently stated being 19. A BMI nearing 15 is usually used as an indicator for starvation and the health risks involved, with a BMI <17.5 being an informal criterion for the diagnosis of anorexia nervosa.
BMI-for-age
BMI is used differently for children. It is calculated the same way as for adults, but then compared to typical values for other children of the same age. Instead of set thresholds for underweight and overweight, then, the BMI percentile allows comparison with children of the same sex and age. A BMI that is less than the 5th percentile is considered underweight and above the 95th percentile is considered overweight. Children with a BMI between the 85th and 95th percentile are considered to be at risk of becoming overweight.
Recent studies in England have indicated that females between the ages 12 and 16 have a higher BMI than males of the same age by 1.0 kg/m² on average.
International variations
These recommended distinctions along the linear scale may vary from time to time and country to country, making global, longitudinal surveys problematic. In 1998, the U.S. National Institutes of Health brought U.S. definitions into line with World Health Organization guidelines, lowering the normal/overweight cut-off from BMI 27.8 to BMI 25. This had the effect of redefining approximately 30 million Americans, previously "technically healthy" to "technically overweight". It also recommends lowering the normal/overweight threshold for South East Asian body types to around BMI 23, and expects further revisions to emerge from clinical studies of different body types.
In Singapore, the BMI cut-off figures were revised in 2005 with an emphasis on health risks instead of weight. Adults whose BMI is between 18.5 and 22.9 have a low risk of developing heart disease and other health problems such as diabetes. Those with a BMI between 23 and 27.4 are at moderate risk while those with a BMI of 27.5 and above are at high risk of heart disease and other health problems.
| Category | BMI range - kg/m2 |
|---|---|
| Starvation | less than 14.9 |
| Underweight | from 15 to 18.4 |
| Normal | from 18.5 to 22.9 |
| Overweight | from 23 to 27.5 |
| Obese | from 27.6 to 40 |
| Morbidly Obese | greater than 40 |
Applications
Statistical device
The Body Mass Index is generally used as a means of correlation between groups related by general mass and can serve as a vague means of estimating adiposity. The duality of the Body Mass Index is that, whilst easy-to-use as a general calculation, it is limited in how accurate and pertinent the data obtained from it can be. Generally, the Index is suitable for recognising trends within sedentary or overweight individuals because there is a smaller margin for errors.
This general correlation is particularly useful for consensus data regarding obesity or various other conditions because it can be used to build a semi-accurate representation from which a solution can be stipulated, or the RDA for a group can be calculated. Similarly, this is becoming more and more pertinent to the growth of children, due to the majority of their exercise habits.
The growth of children is usually documented against a BMI-measured growth chart. Obesity trends can be calculated from the difference between the child's BMI and the BMI on the chart. However, this method again falls prey to the obstacle of body composition: many children who primarily grow as endomorphs would be classed as obese despite body composition. Clinical professionals should take into account the child's body composition and defer to an appropriate technique such as densitometry e.g. Dual energy X-ray absorptiometry, also known as DEXA or DXA.
Clinical practice
BMI has been used by the WHO as the standard for recording obesity statistics since the early 1980s. In the United States, BMI is also used as a measure of underweight, owing to advocacy on behalf of those suffering with eating disorders, such as anorexia nervosa and bulimia nervosa.
BMI can be calculated quickly and without expensive equipment. However, BMI categories do not take into account many factors such as frame size and muscularity. The categories also fail to account for varying proportions of fat, bone, cartilage, water weight, and more.
Despite this, BMI categories are regularly regarded as a satisfactory tool for measuring whether sedentary individuals are "underweight," "overweight" or "obese" with various qualifications, such as: Individuals who are not sedentary being exempt - athletes, children, the elderly, the infirm, and individuals who are naturally endomorphic or ectomorphic (i.e., people who don't have a medium frame).
One basic problem, especially in athletes, is that muscle is denser than fat. Some professional athletes are "overweight" or "obese" according to their BMI - unless the number at which they are considered "overweight" or "obese" is adjusted upward in some modified version of the calculation. In children and the elderly, differences in bone density and, thus, in the proportion of bone to total weight can mean the number at which these people are considered underweight should be adjusted downward.
Medical underwriting
In the United States, where medical underwriting of private health insurance plans is often used, most private health insurance providers will use a particular high BMI as a cut-off point in order to raise insurance rates for or deny insurance to higher-risk patients, thereby ostensibly reducing the cost of insurance coverage to all other subscribers in a 'normal' BMI range. The cutoff point is determined differently for every health insurance provider and different providers will have vastly different ranges of acceptability. Many will implement phased surcharges, in which the subscriber will pay an additional penalty, usually as a percentage of the monthly premium, for each arbitrary range of BMI points above a certain acceptable limit, up to a maximum BMI past which the individual will simply be denied admissibility regardless of price. This can be contrasted with group insurance policies which do not require medical underwriting and where insurance admissibility is guaranteed by virtue of being a member of the insured group, regardless of BMI or other risk factors that would likely render the individual inadmissible to an individual health plan.
Limitations and shortcomings
The medical establishment has generally acknowledged some shortcomings of BMI. Because the BMI is dependent only upon weight and height, it makes simplistic assumptions about distribution of muscle and bone mass, and thus may overestimate adiposity on those with more lean body mass (e.g. athletes) while underestimating adiposity on those with less lean body mass (e.g. the elderly). For example Lance Armstrong was classified as "overweight" when he competed in the 1993 Tour de France.
The exponent of 2 in the denominator of the formula for BMI is arbitrary. It is meant to reduce variability in the BMI associated only with a difference in size, rather than with differences in weight relative to one's ideal weight. If taller people were simply scaled-up versions of shorter people, the appropriate exponent would be 3, as weight would increase with the cube of height. However, on average, taller people have a slimmer build relative to their height than do shorter people, and the exponent which matches the variation best is between 2 and 3. An analysis based on data gathered in the USA suggested an exponent of 2.6 would yield the best fit. The exponent 2 is used instead by convention and for simplicity.
Some argue that the error in the BMI is significant and so pervasive that it is not generally useful in evaluation of health. Due to these limitations, body composition for athletes is often better calculated using measures of body fat, as determined by such techniques as skinfold measurements or underwater weighing and the limitations of manual measurement have also led to new, alternative methods to measure obesity, such as the body volume index. However, recent studies of American football linemen who undergo intensive weight training to increase their muscle mass show that they frequently suffer many of the same problems as people ordinarily considered obese, notably sleep apnea.
In an analysis of 40 studies involving 250,000 people, heart patients with normal BMIs were at higher risk of death from cardiovascular disease than people whose BMIs put them in the "overweight" range (BMI 25-29.9). Patients who were underweight (BMI <20) or severely obese (BMI >35) did, however, have an increased risk of death from cardiovascular disease. The implications of this finding can be confounded by the fact that many chronic diseases, such as diabetes, can cause weight loss before the eventual death. In light of this, higher death rates among thinner people would be the expected result.
A further limitation relates to loss of height through aging. In this situation, BMI will increase without any corresponding increase in weight.