Vaccination
2008/9 Schools Wikipedia Selection. Related subjects: Health and medicine
Vaccination is the administration of antigenic material (the Vaccine) to produce immunity to a disease. Vaccines can prevent or ameliorate the effects of infection by a pathogen. The material administrated can either be live, but weakened forms of pathogens such as bacteria or viruses, killed or inactivated forms of these pathogens, or purified material such as proteins. Smallpox was the first disease people tried to prevent by purposely inoculating themselves with other types of infections; smallpox inoculation was started in India or China before 200 BC. In 1718, Lady Mary Wortley Montague reported that the Turks have a habit of deliberately inoculating themselves with fluid taken from mild cases of smallpox and she inoculated her own children.Before Edward Jenner tested the possibility of using the cowpox vaccine as an immunisation for smallpox in humans in 1796 for the first time, at least six people had done the same several years earlier: a person whose identity is unknown, England, (about 1771), Mrs. Sevel, Germany (about 1772), Mr. Jensen, Germany (about 1770), Benjamin Jesty, England, in 1774, Mrs. Rendall, England (about 1782) and Peter Plett, Germany, in 1791. In 1796 Edward Jenner inoculated using cowpox (a mild relative of the deadly smallpox virus). Pasteur and others built on this.
The term vaccination was first used by Edward Jenner an English physician 22 years later, in 1796. Louis Pasteur further adapted in his pioneering work in microbiology. Vaccination (Latin: vacca—cow) is so named because the first vaccine was derived from a virus affecting cows—the relatively benign cowpox virus—which provides a degree of immunity to smallpox, a contagious and deadly disease. In common speech, 'vaccination' and 'immunization' generally have the same colloquial meaning. This distinguishes it from inoculation which uses unweakened live pathogens, although in common usage either is used to refer to an immunization. The word "vaccination" was originally used specifically to describe the injection of smallpox vaccine.
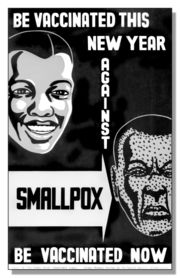
Vaccination efforts have been met with some controversy since their inception, on ethical, political, medical safety, religious, and other grounds. Early success and compulsion brought widespread acceptance and mass vaccination campaigns were undertaken which are credited with greatly reducing the incidence of many diseases in numerous geographic regions. The eradication of smallpox, which was last seen in a natural case in 1977, is considered the most evident success of vaccination.
Triggering immune sensitization
In the generic sense, the process of artificial induction of immunity, in an effort to protect against infectious disease, works by 'priming' the immune system with an ' immunogen'. Stimulating immune response, via use of an infectious agent, is known as immunization. Vaccinations involve the administration of one or more immunogens, which can be administered in several forms.
Some modern vaccines are administered after the patient already has contracted a disease, as in the cases of experimental AIDS, cancer and Alzheimer's disease vaccines. Vaccinia given after exposure to smallpox, within the first four days, is reported to attenuate the disease considerably, and vaccination within the first week is known to be beneficial to a degree. The first Rabies immunization was given by Louis Pasteur to a child bitten by a rabid dog, subsequently post-exposure immunization to Rabies has generally been followed by survival. The essential empiricism behind such immunizations is that the vaccine triggers an immune response more rapidly than the natural infection itself.
Most vaccines are given by hypodermic injection as they are not absorbed reliably through the gut. Live attenuated Polio, some Typhoid and Cholera Vaccines are given orally in order to produce immunity based in the bowel.
Types of vaccinations
All vaccinations work by presenting a foreign antigen to the immune system in order to evoke an immune response, but there are several ways to do this. The three main types are as follows:
- An inactivated vaccine consists of virus particles which are grown in culture and then killed using a method such as heat or formaldehyde. The virus particles are destroyed and cannot replicate, but the virus capsid proteins are intact enough to be recognized by the immune system and evoke a response. When manufactured correctly, the vaccine is not infectious, but improper inactivation can result in intact and infectious particles. Since the properly produced vaccine does not reproduce, booster shots are required periodically to reinforce the immune response.
- In an attenuated vaccine, live virus particles with very low virulence are administered. They will reproduce, but very slowly. Since they do reproduce and continue to present antigen beyond the initial vaccination, boosters are required less often. These vaccines are produced by growing the virus in tissue cultures that will select for less virulent strains, or by mutagenesis or targeted deletions in genes required for virulence. There is a small risk of reversion to virulence, this risk is smaller in vaccines with deletions. Attenuated vaccines also cannot be used by immunocompromised individuals.
- A subunit vaccine presents an antigen to the immune system without introducing viral particles, whole or otherwise. One method of production involves isolation of a specific protein from a virus and administering this by itself. A weakness of this technique is that isolated proteins can be denatured and will then bind to different antibodies than the proteins in the virus. A second method of subunit vaccine is the recombinant vaccine, which involves putting a protein gene from the targeted virus into another virus. The second virus will express the protein, but will not present a risk to the patient. This is the type of vaccine currently in use for hepatitis, and it is experimentally popular, being used to try to develop new vaccines for difficult to vaccinate viruses such as Ebola and HIV.
History of vaccinations
The origins of vaccination are surprisingly older than is commonly known. Early forms of vaccinaton were developed in China as early as 200 B.C. The Anatolian Ottoman Turks knew about methods of vaccination about a hundred years before Edward Jenner to whom the discovery is attributed. They called vaccination Ashi or engrafting, which they used to apply to their children with cowpox taken from the breast of cattle. This kind of vaccination and other forms of variolation were introduced into England by Lady Montagu, a famous English letter-writer and wife of the English ambassador at Istanbul between 1716 and 1718. She came across the Turkish methods of vaccination, consenting to have her son inoculated by the Embassy surgeon Charles Maitland in the Turkish way. Lady Montagu wrote to her sister and friends in England describing the process in details. On her return to England she continued to propagate the Turkish tradition of vaccination and had many of her relatives inoculated. The breakthrough came when a scientific description of the vaccination operation was submitted to the Royal Society in 1724 by Dr Emmanual Timoni, who had been the Montagu’s family physician in Istanbul. Inoculation was adopted both in England and in France nearly half a century before Jenner's famous smallpox vaccine of 1796.
Since then vaccination campaigns have spread throughout the globe, sometimes prescribed by law or regulations (See Vaccination Acts). Vaccines are now used to fight a wide variety of disease threats besides smallpox. Louis Pasteur further developed the technique during the 19th century, extending its use to protecting against bacterial anthrax and viral rabies. The method Pasteur used entailed treating the infectious agents for those diseases so they lost the ability to cause serious disease. Pasteur adopted the name vaccine as a generic term in honour of Jenner's discovery, which Pasteur's work built upon.
Prior to vaccination with cowpox, the only known protection against smallpox was inoculation or variolation (Variola - the Smallpox viruses) where a small amount of live smallpox virus was administered to the patient; this carried the serious risk that the patient would be killed or seriously ill. The death rate from variolation was reported to be around a tenth of that from natural infection with Variola, and the immunity provided was considered quite reliable. Factors contributing to the efficacy of variolation probably include the choices of Variola Minor strains used, the relatively low number of cells infected in the first phase of multiplication following initial exposure, and the exposure route used, via the skin or nasal lining rather than inhalation of droplets into the lungs.
Consistency would suggest the activity should have predated Jenner's description of an effective vaccination system, and there is some history relating to opposition to the older and more hazardous procedure of variolation.
In modern times, the first vaccine-preventable disease targeted for eradication was smallpox. The World Health Organization (WHO) coordinated the global effort to eradicate this disease. The last naturally occurring case of smallpox occurred in Somalia in 1977.
In 1988, the governing body of WHO targeted polio for eradication by the year 2000. Although the target was missed, eradication is very close. The next eradication target would most likely be measles, which has declined since the introduction of measles vaccination in 1963.
In 2000, the Global Alliance for Vaccines and Immunization was established to strengthen routine vaccinations and introduce new and under-used vaccines in countries with a per capita GDP of under US$1000. GAVI is now entering its second phase of funding, which extends through 2014.
Vaccination policies, compulsory vaccination
In an attempt to eliminate the risk of outbreaks of some diseases, at various times several governments and other institutions have instituted policies requiring vaccination for all people. For example, an 1853 law required universal vaccination against smallpox in England and Wales, with fines levied on people who did not comply. Common contemporary U.S. vaccination policies require that children receive common vaccinations before entering school. A few other countries also have some compulsory vaccinations.
Beginning with early vaccination in the nineteenth century, these policies led to resistance from a variety of groups, collectively called anti-vaccinationists, who objected on ethical, political, medical safety, religious, and other grounds. Common objections are that compulsory vaccination represents excessive government intervention in personal matters, or that the proposed vaccinations are not sufficiently safe. Many modern vaccination policies allow exemptions for people who have compromised immune systems, allergies to the components used in vaccinations or strongly-held objections.
Herd immunity and medical risk management issues
Vaccination campaigns are generally accepted as having contributed to the worldwide elimination of smallpox, through herd immunity, and to the restriction of polio to isolated pockets in countries where healthcare access is difficult. The risk management practices of government health agencies' promoting widespread vaccination campaigns has prompted increasing controversy in recent years, despite the fact that many once-common childhood diseases, such as mumps, measles and rubella, are now relatively rare in developed countries.
Adjuvants and preservatives
Vaccines typically contain one or more adjuvants, used to boost the immune response. Tetanus toxoid, for instance, is usually adsorbed onto alum. This presents the antigen in such a way as to produce a greater action than the simple aqueous tetanus toxoid. People who get an excessive reaction to adsorbed tetanus toxoid may be given the simple vaccine when time for a booster occurs.
In the preparation for the 1990 Gulf campaign, Pertussis vaccine (not acellular) was used as an adjuvant for Anthrax vaccine. This produces a more rapid immune response than giving only the Anthrax, which is of some benefit if exposure might be imminent.
They may also contain preservatives, which are used to prevent contamination with bacteria or fungi. Until recent years, the preservative thiomersal was used in many vaccines that did not contain live virus. As of 2005, the only childhood vaccine in the U.S. that contains thiomersal in greater than trace amounts is the influenza vaccine , which is currently recommended only for children with certain risk factors. The UK is considering Influenza immunisation in children perhaps as soon as in 2006-7. Single-dose Influenza vaccines supplied in the UK do not list Thiomersal (its UK name) in the ingredients. Preservatives may be used at various stages of production of vaccines, and the most sophisticated methods of measurement might detect traces of them in the finished product, as they may in the environment and population as a whole .
Combined vaccines
Combined vaccinations are now widely used around the world, a result of the rapid increase in the number of shots recommended in current vaccination schedules.
Methods of administration
A vaccine administration may be oral, by injection (intramuscular, intradermal, subcutaneous), by puncture, transdermal or intranasal.
Vaccine research
Some major contemporary research in vaccination focuses on development of vaccinations for diseases including HIV and malaria.
Vaccine is an international peer-reviewed journal for vaccination researchers, indexed in Medline pISSN: 0264-410X.