Alzheimer's disease
2008/9 Schools Wikipedia Selection. Related subjects: Health and medicine
| Alzheimer's disease Classification and external resources |
|
| Histopathologic image of senile plaques seen in the cerebral cortex in a patient with Alzheimer disease of presenile onset. Silver impregnation. | |
| ICD- 10 | G 30., F 00. |
| ICD- 9 | 331.0, 290.1 |
| OMIM | 104300 |
| DiseasesDB | 490 |
| MedlinePlus | 000760 |
| eMedicine | neuro/13 |
| MeSH | D000544 |
Alzheimer's disease (AD), also called Alzheimer disease or simply Alzheimer's, is the most common type of dementia. Alzheimer's is a degenerative and terminal disease for which there is no known cure. In its most common form, it afflicts individuals over 65 years old, although a less prevalent early-onset form also exists. It is estimated that 26.6 million people worldwide were afflicted by AD in 2006, which could quadruple by 2050, although estimates vary greatly. The disease was first described by Alöis Alzheimer in 1901.
Each individual experiences the symptoms of Alzheimer's disease in unique ways. Generally, the symptoms are reported to a physician when memory loss becomes apparent. If AD is suspected as the cause, the physician or healthcare specialist may confirm the diagnosis with behavioural assessments and cognitive tests, often followed by a brain scan, if available. The prognosis for an individual patient is difficult to assess, as the duration of the disease varies. AD develops for an indeterminate period of time before becoming fully apparent, and it can progress undiagnosed for years. The mean life expectancy following diagnosis is approximately seven years, while fewer than three percent of patients live more than fourteen years. In the early stages, the most commonly recognised symptom is memory loss, such as the difficulty to remember recently learned facts. Earliest occurring symptoms are often mistaken as being noncritical age-related complaints, or forms of stress. As the disease advances, symptoms include confusion, anger, mood swings, language breakdown, long-term memory loss, and the general withdrawal of the sufferer as his or her senses decline. Gradually, minor and major bodily functions are lost, leading ultimately to death.
The cause and progression of Alzheimer's disease are not well understood. Research indicates that the disease is associated with plaques and tangles in the brain. Currently used treatments offer small symptomatic benefit. Many preventive measures have been suggested for Alzheimer's disease, but their value is unproven in reducing the course and severity of the disease. Mental stimulation, exercise and a balanced diet are often recommended, both as a possible prevention and as a sensible way of managing the disease. As of 2008, more than 400 pharmaceutical treatments for AD were being investigated but is unknown if any of them will prove successful.
Because AD cannot be cured and is degenerative, management of the Alzheimer's patient is essential. The role of the main caregiver is often taken by the spouse or a close relative. Alzheimer's disease is known for placing a great burden on caregivers, and the pressures can be wide-ranging, including social, psychological, physical and economic elements of the caregiver's life. AD is one of the most economically expensive diseases to society.
Characteristics
The disease course is divided into four stages, with a progressive pattern of cognitive and functional impairment expressed from one stage to the next and during each stage.
Predementia
Earliest occurring symptoms are often mistaken as being noncritical age-related complaints, or forms of stress. Detailed neuropsychological testing can reveal mild cognitive difficulties up to eight years before a person fulfills the clinical criteria of diagnosis of AD. These early symptoms can have an effect on the most complex daily living activities. The most noticeable deficit is memory loss, shown as a difficulty to remember recently learned facts and an inability to acquire new information. Subtle executive function problems, such as attentiveness, planning, flexibility, or abstract thinking, or impairments in semantic memory, memory of meanings and concept relationships, can also be symptomatic of early stages of AD. Apathy can be observed at this stage and is the most persistent neuropsychiatric symptom throughout the course of the disease. This stage of the disease has also been termed mild cognitive impairment, but there is still a debate on whether this term corresponds to a different diagnostic entity by itself or just a first step of the disease.
Early dementia
In patients with AD, the increasing impairment of learning and memory will lead to a definitive diagnosis. In a small proportion of these patients, difficulties with language, executive functions, recognition of perceptions ( agnosia) or execution of movements ( apraxia) will be more prominent. AD does not affect all memory capacities equally. Older memories of the patient's life ( episodic memory), facts learned ( semantic memory), and implicit memory (the memory of the body on how to do things, such as using a fork to eat) are affected to a much lesser degree than the capacities needed to learn new facts or make new memories. Language problems are mainly characterised by a shrinking vocabulary and a decreased word fluency which leads to a general impoverishment of oral and written language. The Alzheimer's patient is usually capable of adequately communicating basic ideas. While performing fine motor tasks such as writing, drawing or dressing, certain movement coordination and planification difficulties, or apraxia, may be present, which may appear as clumsiness. As the disease progresses to the middle stage, patients can perform tasks independently, but may need assistance or supervision with the most complicated activities.
Moderate dementia
During the early stage, people with AD can usually care for themselves, but progressive deterioration hinders patient independence. Speech difficulties become clearly noticeable due to an inability to recall vocabulary. The patient makes frequent incorrect substitutions ( paraphasias). Reading and writing skills are also progressively lost. As time passes, complex motor sequences become less coordinated, reducing the ability to perform most daily-living activities. During this phase, memory problems worsen, and the person may not recognize close relatives. Long-term memory, which was previously left intact, becomes impaired. At this stage, behaviour changes are more prevalent. Common neuropsychiatric manifestations are irritability and labile affect, leading to crying or outbursts of unpremeditated aggression and physical violence, even in patients whose life-long behaviour has been peaceful. Approximately 30% of the patients also develop illusionary misidentifications and other delusional symptoms. Urinary incontinence can develop. Because of the communication deficit along with delusions, patients often resist when caregivers attempt to provide care. All these symptoms create stress for relatives and caretakers, increasing the likelihood of moving the patient from home care to other long-term care facilities.
Advanced
During this last stage of AD, the patient is completely dependent upon caregivers. Language is reduced to simple phrases or even single words, eventually leading to complete loss of speech. Despite the loss of verbal language abilities, patients can receive and return emotional signals. Although aggressiveness can still be present, extreme apathy and exhaustion are much more common results. Patients will ultimately not be able to perform even the most simple tasks without assistance. Muscle mass and mobility will deteriorate to the point where the patient is bedridden, and they will also lose the ability to feed themselves. Death occurs from some external factor such as pressure ulcers or pneumonia, and not from the disease itself.
Causes
Three major competing hypotheses exist to explain the cause of the disease. The oldest, on which most currently available drug therapies are based, is known as the cholinergic hypothesis and suggests that AD is due to reduced biosynthesis of the neurotransmitter acetylcholine. The medications that treat acetylcholine deficiency only affect symptoms of the disease and neither halt nor reverse it. The cholinergic hypothesis has not maintained widespread support in the face of this evidence, although cholinergic effects have been proposed to initiate large-scale aggregation, leading to generalised neuroinflammation.
In 1991, the amyloid hypothesis was proposed, which states that amyloid beta (Aβ) deposits are the causative factor in the disease. In a recent study, an experimental vaccine was found to have cleared patients of plaques but did not have any significant effect on their dementia, which contradicts the predictions of the amyloid hypothesis.
Research has focused on tau protein abnormalities that initiate the disease cascade. The tau hypothesis is supported by the long-standing observation that deposition of amyloid plaques does not correlate well with neuron loss. In this model, hyperphosphorylated tau begins to pair with other threads of tau. Eventually, they become tangled inside nerve cell bodies, forming what are known as neurofibrillary tangles. When this occurs, the microtubules disintegrate, collapsing the neuron's transport system. This may result first in malfunctions in biochemical communication between neurons and later in the death of the cells.
A majority of researchers support the alternative hypothesis that Aβ is the primary causative agent. The amyloid hypothesis is compelling because the gene for the amyloid beta precursor (APP) is located on chromosome 21, and patients with trisomy 21 (Down Syndrome) who thus have an extra gene copy almost universally exhibit AD-like disorders by 40 years of age. It should be noted further that APOE4, the major genetic risk factor for AD, leads to excess amyloid build-up in the brain before AD symptoms arise. Thus, Aβ deposition precedes clinical AD. It is known that some types of inherited AD involve only mutations in the APP gene (although this is not the most common type—others involve genes for "pre-senilin" proteins which process APP and may also have still-unknown functions). However, another strong support for the amyloid hypothesis, which looks at Aβ as the common initiating factor for Alzheimer's disease, is that transgenic mice solely expressing a mutant human APP gene develop fibrillar amyloid plaques.
Pathophysiology
Neuropathology
At a macroscopic level, AD is characterised by loss of neurons and synapses in the cerebral cortex and certain subcortical regions. This results in gross atrophy of the affected regions, including degeneration in the temporal lobe and parietal lobe, and parts of the frontal cortex and cingulate gyrus.
Both amyloid plaques and neurofibrillary tangles are clearly visible by microscopy in AD brains. Plaques are dense, mostly insoluble deposits of amyloid-beta protein and cellular material outside and around neurons that build up to insoluble twisted fibers within the nerve cell, often called tangles. Though many older people develop some plaques and tangles, the brains of AD patients have them to a much greater extent and in different brain locations.
Biochemical characteristics
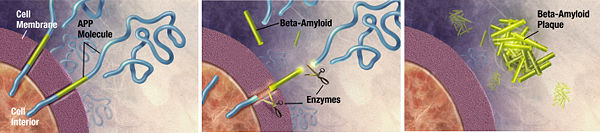
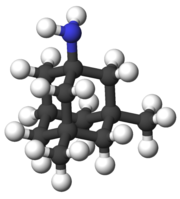
Alzheimer's disease has been identified as a protein misfolding disease, or proteopathy, due to the accumulation of abnormally folded A-beta and tau proteins in the brains of AD patients. Plaques are made up of small peptides (39 to 43 amino acid residues each) called beta-amyloid (also written as A-beta or Aβ), a protein fragment from a larger protein called amyloid precursor protein (APP). APP is a transmembrane protein, which sticks through the neuron's membrane, and helps neurons grow, survive and repair themselves after injury. In AD, an unknown process causes APP to be divided into smaller fragments by enzymes through proteolysis. One of these fragments is beta-amyloid, or amyloid fibrils, which form clumps that deposit outside neurons in dense formations known as senile plaques.
AD is also considered a tauopathy due to abnormal aggregation of the tau protein. Healthy neurons have an internal support structure, or cytoskeleton, partly made up of structures called microtubules. These microtubules act like tracks, guiding nutrients and molecules from the body of the cell down to the ends of the axon and back. A protein called tau makes the microtubules stable when phosphorylated, and is therefore called a microtubule-associated protein. In AD, tau is changed chemically, becoming hyperphosphorylated, causing microtubules to disintegrate.
Disease mechanism
The exact mechanism of how the production and aggregation of the amyloid beta peptide plays a key role in AD has not been elucidated. The traditional formulation of the amyloid hypothesis points to the accumulation of beta-amyloid peptides as the central event triggering neuron degeneration. Accumulation of aggregated amyloid fibrils, which are believed to be the toxic form of the protein responsible for disrupting the cell's calcium ion homeostasis, induces apoptosis, or programmed cell death. It is also known that Aβ selectively builds up in the mitochondria in the cells of brains with AD, and it also inhibits certain enzyme functions and the utilization of glucose by neurons. This process may also lead to the formation of damaging reactive oxygen species, calcium influx, and apoptosis.
Various inflammatory processes and cytokines may also have a role in the pathology of Alzheimer's disease. These inflammations are general markers of tissue damage in any disease, and may be either secondary causes of tissue damage in AD or else bystander marker effects from an immunological response.
Genetic
While earlier disease familial onset is mainly explained by three genes, later age of disease onset representing most cases of AD has yet to be explained by a purely genetic model. In the second case the APOE gene is the strongest genetic risk factor discovered but it is far from explaining all occurrences of the disease.
Only 10% of AD cases occurring before 60 years of age are due to autosomal dominant (familial) mutations, which represents less than 0,01 of all patients. These mutations have been discovered in three different genes: amyloid precursor protein or APP, and presenilins 1, and 2. Most mutations in the APP and presenilin genes increase the production of a small protein called Abeta42, which is the main component of senile plaques in brains of AD patients.
Most cases of Alzheimer's disease do not exhibit familial inheritance. In this case genes may act as risk factors. The best known genetic risk factor is the inheritance of the ε4 allele of the apolipoprotein E (APOE). This gene is regarded as a risk factor for development of up to 50% of late-onset sporadic Alzheimer's. Genetic experts agree that there are other risk and protective factor genes that influence the development of late onset Alzheimer's disease. Over 400 genes have been tested for association with late-onset sporadic AD.
Diagnosis
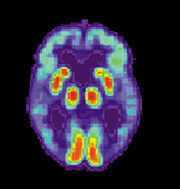
Dementia is by definition a clinical condition but not an exact diagnosis. Alzheimer's disease is usually diagnosed clinically from the patient history, collateral history from relatives, and clinical observations, based on the presence of characteristic neurological and neuropsychological features and the absence of alternative conditions. Advanced medical imaging with CT (Computed tomography) or MRI (Magnetic resonance imaging), and with SPECT (Single photon emission computed tomography) or PET (Positron emission tomography) are generally used to help to diagnose the subtype of dementia and exclude other cerebral pathology. Assessment of intellectual functioning including memory testing can further characterize the dementia. Medical organizations have created diagnostic criteria to ease and standardize the process for practicing physicians. Sometimes the diagnosis can be confirmed or made at postmortem when brain material is available and can be examined histologically.
Diagnostic criteria
The diagnostic criteria for Alzheimer of the NINCDS-ADRDA ( NINCDS and the ADRDA) are among the most used. These criteria require that the presence of cognitive impairment and a suspected dementia syndrome be confirmed by neuropsychological testing for a clinical diagnosis of possible or probable AD while they need histopathologic confirmation ( microscopic examination of brain tissue) for the definitive diagnosis. They have shown good reliability and validity. They specify as well eight cognitive domains that may be impaired in AD (i.e., memory, language, perceptual skills, attention, constructive abilities, orientation, problem solving and functional abilities). Similar to the NINCDS-ADRDA Alzheimer's Criteria are the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) criteria published by the American Psychiatric Association.
Diagnostic tools
Neuropsychological screening tests such as the Mini mental state examination (MMSE) are widely used to evaluate the cognitive impairments needed for diagnosis, but more comprehensive tests arrays are necessary for high reliability by this method, especially in the earliest stages of the disease. Neurological examination in early AD will usually be normal, independent of cognitive impairment; but for many of the other dementing disorders is key for diagnosis. Therefore, neurological examination is crucial in the differential diagnosis of AD and other diseases. In addition, interviews with family members are also utilized in the assessment of the disease. Caregivers can supply important information on the daily living abilities, as well as on the decrease over time of the patient's mental function. This is especially important since a patient with AD is commonly unaware of his or her own deficits ( anosognosia). Many times families also have difficulties in the detection of initial dementia symptoms and in adequately communicating them to a physician. Finally, supplemental testing provides extra information on some features of the disease or are used to rule out other diagnoses. Examples are blood tests, which can identify other causes for dementia different than AD, which rarely may even be reversible; or psychological tests for depression, as depression can both co-occur with AD or, on the contrary, be at the origin of the patient's cognitive impairment.
Increasingly, the functional neuroimaging modalities of single photon emission computed tomography (SPECT) and positron emission tomography (PET) are being used to diagnose Alzheimer's, as they have shown similar ability to diagnose Alzheimer's disease as methods involving mental status examination. Furthermore, the ability of SPECT to differentiate Alzheimer's disease from other possible causes, in a patient already known to be suffering from dementia, appears to be superior to attempts to differentiate the cause of dementia cause by mental testing and history. A new technique known as "PiB PET" has been developed for directly and clearly imaging beta-amyloid deposits in vivo using a contrasting tracer that binds selectively to the Abeta deposits. Another recent objective marker of the disease is the analysis of cerebrospinal fluid for amyloid beta or tau proteins. Both advances (neuroimaging and cerebrospinal fluid analysis) have led to the proposal of new diagnostic criteria.
Prevention
At present, contradictory results in global studies, incapacity to prove causal relationships between risk factors and the disease, and possible secondary effects indicate a lack of specific measures to prevent or delay the onset of AD. Different epidemiological studies have proposed relationships between certain modifiable factors, such as diet, cardiovascular risk, pharmaceutical products, or intellectual activities among others, and a population's likelihood of developing AD. Only further research, including clinical trials, will reveal whether, in fact, these factors can help to prevent AD.
The components of a Mediterranean diet, which include fruit and vegetables, bread, wheat and other cereals, olive oil, fish, and red wine, may all individually or together reduce the risk and course of Alzheimer's disease. Vitamins B and C, or folic acid have appeared to be related to a reduced risk of AD, but other studies indicate that they do not have any significant effect on the onset or course of the disease and may have important secondary effects. Curcumin in curry has shown some effectiveness in preventing brain damage in mouse models.
Although cardiovascular risk factors, such as hypercholesterolemia, hypertension, diabetes, and smoking, are associated with a higher risk of onset and course of AD, statins, which are cholesterol lowering drugs, have not been effective in preventing or improving the course of the disease. However long-term usage of non-steroidal anti-inflammatory drug (NSAIDs), is associated with a reduced likelihood of developing AD in some individuals. Other pharmaceutical therapies such as female hormone replacement therapy are no longer thought to prevent dementia, and a 2007 systematic review concluded that there was inconsistent and unconvincing evidence that ginkgo has any positive effect on dementia or cognitive impairment.
Intellectual activities such as playing chess, completing crossword puzzles or regular social interaction, may also delay the onset or reduce the severity of Alzheimer's disease. Bilingualism is also related to a later onset of Alzheimer's.
Some studies have shown a positive relationship between risk of developing AD and different occupational exposures such as magnetic field exposure,, metals intake and specifically aluminium, or solvents. The quality of some of these studies has been criticized, and other research does not confirm this link.
Management
There is no known cure for Alzheimer's disease. Available treatments offer relatively small symptomatic benefit but remain palliative in nature. Current treatments can be divided into pharmaceutical, psychosocial and caregiving.
Pharmaceutical
Four medications, to treat the cognitive manifestations of AD, are currently approved by regulatory agencies, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMEA). Three are acetylcholinesterase inhibitors and the other is memantine, an NMDA receptor antagonist. No drug has an indication for delaying or halting the progression of the disease.
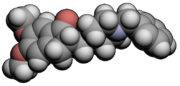
Because reduction in the activity of the cholinergic neurons in the disease is well known, acetylcholinesterase inhibitors are employed to reduce the rate at which acetylcholine (ACh) is broken down and so to increase the concentration of ACh in the brain, thereby combatting the loss of ACh caused by the death of the cholinergic neurons. Cholinesterase inhibitors currently approved include donepezil (brand name Aricept), galantamine (Razadyne), and rivastigmine (branded as Exelon, and Exelon Patch). There is evidence for the efficacy of these medications in mild to moderate Alzheimer’s disease, and some evidence for their use in the advanced stage. Only donepezil is approved for treatment of advanced AD dementia. The use of these drugs in mild cognitive impairment has not shown any effect in a delay of the onset of AD. Most common side effects include nausea and vomiting, both of which are linked to cholinergic excess. These side effects arise in approximately ten to twenty percent of users and are mild to moderate in severity. Less common secondary effects include muscle cramps; decreased heart rate ( bradycardia), decreased appetite and weight, and increased gastric acid.
Glutamate is a useful excitatory neurotransmitter of the nervous system, although excessive amounts in the brain can lead to cell death through a process called excitotoxicity which consists of the overstimulation of glutamate receptors. Excitotoxicity occurs not only in Alzheimer's disease, but also in other neurological diseases such as Parkinson's disease and multiple sclerosis. Memantine (brand names Akatinol, Axura, Ebixa/Abixa, Memox and Namenda), is a noncompetitive NMDA receptor antagonist first used as an anti-influenza agent. It acts on the glutamatergic system by blocking NMDA glutamate receptors and inhibits their overstimulation by glutamate. Memantine has been shown to be moderately efficacious in the treatment of moderate to severe Alzheimer’s disease. Its effects in the initial stages are unknown. Reported adverse events with memantine are infrequent and mild, including hallucinations, confusion, dizziness, headache and fatigue. Memantine used in combination with donepezil has been shown to be "of statistically significant but clinically marginal effectiveness".
Neuroleptic anti-psychotic drugs given to Alzheimer's patients with behavioural problems are modestly useful in reducing aggression and psychosis, but are associated with serious adverse effects, such as cerebrovascular events, movement difficulties or cognitive decline, that do not permit their routine use.
Psychosocial intervention
Psychosocial interventions are used as an adjunct to pharmaceutical treatment and can be classified within behaviour, emotion, cognition or stimulation oriented approaches. Research on efficacy is unavailable and rarely specific to the disease, focusing instead on dementia.
Behavioural interventions attempt to identify and reduce the antecedents and consequences of problem behaviors. This approach has not shown success in the overall functioning of patients, but can help to reduce some specific problem behaviors, such as incontinence. There is still a lack of high quality data on the effectiveness of these techniques in other behaviour problems such as wandering.
Emotion-oriented interventions include reminiscence therapy, validation therapy, supportive psychotherapy, sensory integration or snoezelen, and simulated presence therapy. Supportive psychotherapy has received little or no formal scientific study, but some clinicians find it useful in helping mildly impaired patients adjust to their illness. Reminiscence therapy (RT) involves the discussion of past experiences individually or in group, many times with the aid of photographs, household items, music and sound recordings, or other familiar items from the past. Although there are few quality studies on the effectiveness of RT it may be beneficial for cognition and mood. Simulated presence therapy (SPT) is based on attachment theories and is normally carried out playing a recording with voices of the closest relatives of the patient. There is preliminary evidence indicating that SPT may reduce anxiety and challenging behaviors. Finally, validation therapy is based on acceptance of the reality and personal truth of another's experience, while sensory integration is based on exercises aimed to stimulate senses. There is little evidence to support the usefulness of these therapies.
The aim of cognition-oriented treatments, which include reality orientation and cognitive retraining is the restoration of cognitive deficits. Reality orientation consists in the presentation of information about time, place or person in order to ease the understanding of the person about its surroundings and his place in them. On the other hand cognitive retraining tries to improve impaired capacities by exercitation of mental abilities. Both have shown some efficacy improving cognitive capacities, although in some works these effects were transient and negative effects, such as frustration, have also been reported.
Stimulation-oriented treatments include art, music and pet therapies, exercise, and any other kind of recreational activities for patients. Stimulation has modest support for improving behaviour, mood, and, to a lesser extent, function. Nevertheless, as important as these effects are, the main support for the use of stimulation therapies is the improvement in the patient daily life routine they suppose.
Caregiving
Since Alzheimer's has no cure and it gradually renders patients incapable of tending for their own needs, caregiving essentially is the treatment and must be carefully managed over the course of the disease.
During the early and moderate stages, modifications to the patient's living environment and lifestyle can increase patient safety and reduce caretaker burden. Examples of such modifications are the adherence to simplified routines, the placing of safety locks, the labeling of household items to cue the patient or the use of modified daily life objects.
As the disease progresses, different medical issues can appear, such as oral and dental disease, pressure ulcers, malnutrition, hygiene problems, or respiratory, skin, or eye infections. Careful management of the patient can prevent them, while professional treatment is needed when they do arise. When swallowing difficulties begin the use of feeding tubes is debated both from an evidence-based and an ethical point of view. The use of physical restraints is rarely indicated in any stage of the disease, although there are situations when they are necessary to prevent harm to the patient or their caregivers. During the final stages of the disease, treatment is centered in relieving discomfort until death.
Prognosis
The early stages of Alzheimer's disease are difficult to diagnose. A definitive diagnosis is usually made once cognitive impairment compromises daily living activities. At this time, the patient will progress from mild cognitive problems, such as memory loss, but still able to live independently, through increasing stages of cognitive and non-cognitive disturbances, eliminating any possibility of independent living.
Life expectancy of the population with the disease is reduced. The mean life expectancy following diagnosis is approximately seven years, while fewer than three percent of patients live more than fourteen years. Disease features significantly associated with reduced survival are an increased severity of cognitive impairment, decreased functional level, history of falls, and disturbances in the neurological examination. The cooccurrence of other diseases such as heart problems, diabetes or history of alcohol abuse are also related with shortened survival. While the earlier the age at onset the higher the total survival years, life expectancy is specially reduced when compared to the healthy population among those who are younger. Regarding sexes men have a less favourable survival prognosis than women.
The disease is the underlying cause of death in 70% of AD patients. Pneumonia and dehydration are the most frequent immediate causes of death, while cancer is a less frequent cause of death than in the general population.
Epidemiology
| Age | Incidence (new affected per 1000 and year) |
|---|---|
| 65–69 | 2 |
| 70–74 | 6 |
| 75–79 | 9 |
| 80–84 | 23 |
| 85–89 | 40 |
| Older than 90 | 69 |
Two main measures are used in epidemiological studies: incidence and prevalence. Incidence is the number of new cases per unit of person-time at risk (usually number of new cases per 1000 and year); while prevalence is the total number of cases of the disease in the population at a given time.
Regarding incidence, cohort longitudinal studies (studies where a disease free population is followed over the years) provide rates between 10–15 per 1000 and year for all dementias and 5–8 for AD; which means that half of new dementia cases each year are AD. Advancing age is a primary risk factor for the disease and incidence rates are not equal for all ages: every five years after the age of 65, the risk of acquiring the disease doubles increasing from 2 per 1000 to as much as 69 per 1000. There are also sex differences in the incidence rates, having women a higher risk of developing AD specially in the population older than 85.
Prevalence depends on different factors including incidence but also patient survival. Since the incidence of AD increases with age it is specially important the mean age of the population of interest. United States specific Alzheimer prevalence was estimated to be 1'6 % in the year 2000.In the age group between 65–74 around 5% of the U.S. population had AD, increasing almost to 20% in the 75–84 group and to 50% afterwards Prevalence rates in less developed countries, such as India or Taiwan, are usually lower. Few studies have tried to make world-wide estimations of Alzheimer's disease prevalence, being much more common estimations of dementia in general. The World Health Organization provided an estimation of approximately 24.5 millions of people affected with any kind of dementia in 2005, which was going to increase to 30 million in 2015 and reach 45 millions by 2030; giving other studies similar numbers. Other study provided a worldwide estimation of Alzheimer in 2006 of 26.6 million which would multiply by four by the year 2050.
History
Although the concept of dementia goes as far back as the ancient Greek and Roman philosophers and physicians, it was in 1901 when Alöis Alzheimer, a German psychiatrist, identified the first case of what became known as Alzheimer's disease in a fifty-year-old woman he called Auguste D. Alöis Alzheimer followed her until she died in 1906, when he first reported the case publicly. In the following five years, eleven similar cases were reported in the medical literature, some of them already using the term Alzheimer's disease. The official consideration of the disease as a distinctive entity is attributed to Emil Kraepelin, who included Alzheimer’s disease or presenile dementia as a subtype of senile dementia in the eighth edition of his Textbook of Psychiatry, published in 1910.
For most of the twentieth century, the diagnosis of Alzheimer's disease was reserved for individuals between the ages of 45 and 65 who developed symptoms of dementia. The terminology changed after 1977 when a conference concluded that the clinical and pathological manifestations of presenile and senile dementia were almost identical, although the authors also added that this did not rule out the possibility of different etiologies. This eventually led to the use of Alzheimer's disease independently of onset age of the disease. The term senile dementia of the Alzheimer type (SDAT) was used for a time to describe the condition in those over 65, with classical Alzheimer's disease being used for those younger. Eventually, the term Alzheimer's disease was formally adopted in medical nomenclature to describe individuals of all ages with a characteristic common symptom pattern, disease course, and neuropathology.
Society and culture
Social costs
Dementia, and specifically Alzheimer's disease may be among the most costly diseases for society in the developed countries, while their cost in developing countries such as Argentina, or Korea, is also high and rising. These costs will probably increase with the aging of society, becoming an important social problem. AD associated costs include direct medical costs such as nursing home care, direct nonmedical costs such as in-home day care, and indirect costs such as lost patient and caregiver productivity. Numbers vary between studies but dementia costs worldwide have been calculated around $160 billion, while costs of Alzheimer in the United States may be $100 billion each year.
The greatest origin of costs for society is the long-term care by health care professionals and specially institutionalization; which corresponds to 2/3 of the total costs for society. The cost of living at home is also very high, specially when informal costs for the family, such as caregiving time and caregiver's lost earnings are taken into account. However it still seems lower to institutionalization.
Costs increase with dementia severity and the presence of behavioural disturbances, and are related to the increased caregiving time required for the provision of physical care. Therefore any treatment that slows cognitive decline, delays instituzionalization or reduces caregivers hours will have economic benefits. Economic evaluations of current treatments have shown positive results.
Caregiving burden
The role of the main caregiver is often taken by the spouse or a close relative. Alzheimer's disease is known for placing a great burden on caregivers which includes social, psychological, physical or economic aspects. Home care is usually preferred by patients and families. This option also delays or eliminates the need for more professional and costly levels of care. Nevertheless two-thirds of nursing home residents have dementias.
Dementia caregivers are subject to high rates of physical and mental disorders. Factors associated with greater psychosocial problems of the primary caregivers include having an affected person at home, the carer being a spouse, demanding behaviors of the patient such as depression, behavioural disturbances, hallucinations, sleep problems or walking disruptions and social isolation. Regarding economic problems, family caregivers often give up time from work to spend 47 hours per week on average with the person with AD, while the costs of caring an Alzheimer's patient are high. Direct and indirect costs of caring for an Alzheimer's patient average between $18,000 and $77,500 per year and patient in the United States, depending on the study.
Individual behavioural therapy and the teaching coping strategies either individually or in group have both demonstrated their efficacy improving caregivers psychological health. Nevertheless caregiving can also have some positive effects in main carers.
Notable cases
As a result of the prevalence of the disease, many notable people have contracted it. Well-known examples are former United States President Ronald Reagan and Irish writer Iris Murdoch, both of whom have scientific articles on how their cognitive capacities deteriorated with the disease. Other cases include the retired footballer Ferenc Puskas, the former British Prime Minister Harold Wilson, the actress Rita Hayworth, the actor Charlton Heston, and the novelist Terry Pratchett.
Alzheimers has also been portrayed in films such as: Iris (2001), (based on John Bayley's memoir of his wife Iris Murdoch); The Notebook (2004), (based on Nicholas Sparks' 1996 novel of the same name); Thanmathra (2005); Memories of Tomorrow (Ashita no Kioku) (2006), (based on Hiroshi Ogiwara's novel of the same name); and Away from her (2006), (based on Alice Munro's short story The bear came over the mountain). Documentaries on AD include Malcolm and Barbara: A Love Story (1999) and Malcolm and Barbara: Love’s Farewell (2007), both featuring Malcolm Pointon.
Research directions
As of 2008, the safety and efficacy of more than 400 pharmaceutical treatments are being investigated in clinical trials worldwide, and approximately one-fourth of these compounds are in Phase III trials, which is the last step prior to review by regulatory agencies. It is unknown as to whether any of these trials will ultimately prove successful in treating the disease.
A critical area of clinical research is focused on treating the underlying disease pathology. Reduction of amyloid beta levels is a common target of compounds under investigation. Immunotherapy or vaccination for the amyloid protein is one treatment modality under study. Unlike preventative vaccination, the putative therapy would be used to treat people already diagnosed. It is based upon the concept of training the immune system to recognize, attack, and reverse deposition of amyloid, thereby altering the course of the disease. An example of such a vaccine under investigation was ACC-001, although the trials were suspended in 2008. Similar agents are bapineuzumab, an antibody designed as identical to the naturally-induced anti-amyloid antibody, and MPC-7869, a selective amyloid beta-42 lowering agent. Other approaches are neuroprotective agents, such as AL-108, and metal-protein interaction attenuation agents, such as PBT2. A TNFα receptor fusion protein, etanercept has showed encouraging results.
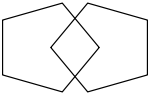
In 2008, researchers announced positive results in modifying the course of disease in mild to moderate AD with methylthioninium chloride (MTC), (trade name rember) a drug that inhibits Tau aggregation, and dimebon, an antihistamine.