HIV/AIDS in Africa
2008/9 Schools Wikipedia Selection. Related subjects: African Geography
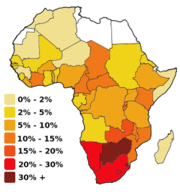
The HIV/AIDS epidemics spreading through the countries of Sub-saharan Africa are highly varied. Although it is not correct to speak of a single African epidemic, Africa is without doubt the region most affected by the virus. Inhabited by just over 12% of the world's population, Africa is estimated to have more than 60% of the AIDS-infected population. Much of the deadliness of the epidemic in Sub-Saharan Africa has to do with a deadly synergy between HIV and Tuberculosis. In fact, Tuberculosis is the world's greatest infectious killer of women of reproductive age and the leading cause of death among people with HIV/AIDS.
| World region | Adult HIV prevalence (ages 15–49) |
Total HIV cases |
AIDS deaths in 2005 |
|---|---|---|---|
| Sub-Saharan Africa | 6.1% | 24.5m | 2.0m |
| Worldwide | 1.0% | 38.6m | 2.8m |
| North America | 0.11% | 1.3m | 27,000 |
| Western Europe | 0.3% | 5.8m | 12,000 |
| Regional comparisons of HIV in 2005 (Source: UNAIDS, 2006 Report on the global AIDS epidemic) |
In Southern Africa, several factors contribute to the spread of the HIV virus. For one, a stigma is attached to admitting to HIV infection and to using condoms. For another, many deny that the HIV virus causes AIDS: Thabo Mbeki and Robert Mugabe have both suggested AIDS stems from poverty rather than HIV infection. And finally, many myths are attached to the use of condoms, such as the ideas that a conspiracy wants to limit the growth of the African population and that condoms stifle the traditional power of the man in his community.
In the 35 African nations with the highest prevalence, average life expectancy is 48.3 years—6.5 years less than it would be without the disease. For the eleven countries in Africa with prevalence rates above 13%, life expectancy is 47.7 years—11.0 years less than would be expected without HIV/AIDS.
Although many governments in sub-Saharan Africa denied that there was a problem for years, they have now begun to work toward solutions.
Health spending in Africa has never been adequate, either before or after independence. The health care systems inherited from colonial powers were oriented toward curative treatment rather than preventative programs. Strong prevention programs are the cornerstone of effective national responses to AIDS, and the required changes in the health sector have presented huge challenges.
Lack of money is an obvious challenge, although a great deal of aid is distributed throughout developing countries with high HIV/AIDS rates. Response to the epidemic is also hampered by lack of infrastructure, corruption within both donor agencies and government agencies, foreign donors not coordinating with local government and misguided resources.
The Joint United Nations Programme on HIV/AIDS (UNAIDS) has predicted outcomes for the region to the year 2025. These range from a plateau and eventual decline in deaths beginning around 2012 to a catastrophic continual growth in the death rate with potentially 90 million cases of infection.
Without the kind of nutrition, health care and medicines (such as anti-retrovirals) that are available in developed countries, large numbers of people in Africa will develop full-blown AIDS. They will not only be unable to work, but will also require significant medical care. This will likely cause a collapse of economies and societies. In all of the severely affected countries, the epidemic has left behind many orphans, who are either cared for by extended family members, or must live in orphanages or on the streets. UNAIDS, WHO and UNDP have already documented decreasing life expectancies and lowering of GNP in many African countries with prevalence rates of 10% or more.
A minority of scientists claim that as many as 40% of HIV infections in African adults may be caused by unsafe medical practices rather than by sexual activity. . The World Health Organization states that 2.5% of infections are caused by unsafe medical injection practices and all the others by unprotected sex. .
Access to treatment
- "Treatment is technically feasible in every part of the world. Even the lack of infrastructure is not an excuse—I don't know a single place in the world where the real reason AIDS treatment is unavailable is that the health infrastructure has exhausted its capacity to deliver it. It's not knowledge that's the barrier. It's political will." Peter Piot, Executive Director of UNAIDS
New anti-retroviral drugs (ARVs) can slow down and even reverse the progression of HIV infection, delaying the onset of AIDS by twenty years or more. Because of their high cost ($10,000 to $15,000 USD per person per year (pppy) in the West for patent drugs and approximately $800 USD pppy in some African countries for generic drugs), only a few of the 6 million people in developing countries who need ARV treatment have access to medication. Nevertheless, access to ARV therapy has increased more than eightfold since the end of 2003, with about 810,000 people (13.5 per cent of the 6 million in need) on the treatment.
ARVs play a central role in prevention as well. When treatments are known to be available, people are more likely to come forward for testing and well as more likely to adopt lower risk behaviours. ARVs also reduce the amount of the HIV virus in the blood, thus reducing the risk of further transmission.
Patients who start HIV treatment generally have to continue taking medications for the rest of their lives. In areas where drug therapy is expensive, some people must interrupt their treatment when they were unable to afford medication. Drug-resistant strains of HIV have been observed in such areas.
The key factor in the expense of ARVs is their patent status, which allows drug companies to recoup research costs and turn a profit, enabling the development of new drugs. International aid organisations such as VSO, Oxfam and Médecins Sans Frontières have questioned whether the revenues generated by ARVs really tally with research costs.
Generic copies of patented ARV drugs are supplied by drug manufacturers in India, South Africa, Brazil, Thailand, and the People's Republic of China. Because fees are not paid to the patent holders, the drugs can be distributed at low prices in developing countries. Generic production competition and 'price offers' (voluntary donations by companies) have forced patent holders to reduce their prices.
ARV patients need regular testing of viral load and CD4 cell count. This requires expensive laboratory equipment and good healthcare logistics. These costs drive the price of generic ARV therapy in African countries up from under $140 USD pppy for the drugs alone to approximately $800 USD pppy when done according to Western standards.
For many Africans, living below the poverty threshold of a $2 USD / day, free (government or NGO-funded) treatment remains the only option.
The World Health Organisation's 3 by 5 initiative aimed to provide three million people with ARV treatment by the end of 2005. International aid organisations have lobbied for an expansion of generic production in developing countries, for immediate short term and stable, predictable long term financing of the 3 by 5 initiative.
The United States AIDS initiative, PEPFAR, is focusing two thirds of its resources on AIDS in Africa. Starting in 2004, expenditures rose from $2.3B world-wide to $3.3B in 2006. A funding level of $4B was requested for 2007.
The DREAM ("Drug Resources Enhancement against AIDS and Malnutrition", formerly "Drug Resource Enhancement against AIDS in Mozambique") initiative promoted by the Community of Sant'Egidio has given access to free ARV treatment with generic HAART drugs to the poor on a large scale. So far, 5,000 people are receiving ARV treatment, especially in Mozambique, but the program is also being built up in Malawi, Guinea, Tanzania and other countries. The program includes regular blood testing according to European standards. It is linked with nutrition and sanitation programs run by volunteers. The compliance rate is 94 per cent.
Regional analysis
East-central Africa
In this article, East and central Africa consists of Uganda, Kenya, Tanzania, Democratic Republic of Congo, the Congo Republic, Gabon, Equatorial Guinea, the Central African Republic, Rwanda, Burundi and Ethiopia and Eritrea on the Horn of Africa. In 1982, Uganda was the first state in the region to declare HIV cases. This was followed by Kenya in 1984 and Tanzania in 1985.
|
||||||||||||||||||||||||||||||||
| HIV in East-central Africa (Source: UNAIDS) * A 2005 survey by the Central Statistical Agency of Ethiopia showed that Adult (ages 15-49) prevalence was only 1.4%, with prevalence among women at 1.9% and among men at 0.9%. |
Some areas of East Africa are beginning to show substantial declines in the prevalence of HIV infection. In the early 1990s, 13% of Ugandan residents were HIV positive; This has now fallen to 4.1% by the end of 2003. Evidence may suggest that the tide may also be turning in Kenya: prevalence fell from 13.6% in 1997–1998 to 9.4% in 2002. Data from Ethiopia and Burundi are also hopeful. HIV prevalence levels still remain high, however, and it is too early to claim that these are permanent reversals in these countries' epidemics.
Most governments in the region established AIDS education programmes in the mid-1980s in partnership with the World Health Organization and international NGOs. These programmes commonly taught the 'ABC' of HIV prevention: a combination of abstinence (A), fidelity to your partner (Be faithful) and condom use (C). The efforts of these educational campaigns appear now to be bearing fruit. In Uganda, awareness of AIDS is demonstrated to be over 99% and more than three in five Ugandans can cite two or more preventative practices. Youths are also delaying the age at which sexual intercourse first occurs.
There are no non-human vectors of HIV infection. The spread of the epidemic across this region is closely linked to the migration of labour from rural areas to urban centres, which generally have a higher prevalence of HIV. Labourers commonly picked up HIV in the towns and cities, spreading it to the countryside when they visited their home. Empirical evidence brings into sharp relief the connection between road and rail networks and the spread of HIV. Long distance truck drivers have been identified as a group with the high-risk behaviour of sleeping with prostitutes and a tendency to spread the infection along trade routes in the region. Infection rates of up to 33% were observed in this group in the late 1980s in Uganda, Kenya and Tanzania.
West Africa
For the purposes of this discussion, Western Africa shall include the coastal countries of Mauritania, Senegal, The Gambia, Cape Verde, Guinea-Bissau, Guinea, Sierra Leone, Liberia, Côte d'Ivoire, Ghana, Togo, Benin, Nigeria and the landlocked states of Mali, Burkina Faso and Niger.
| Country | Adult prevalence | Total HIV | Deaths 2005 |
|---|---|---|---|
| Cote D'Ivoire | 7.1% | 750,000 | 65,000 |
| Liberia | 5.9% | 100,000 | 72,000 |
| Nigeria | 5.4% | 3,600,000 | 310,000 |
| Guinea-Bissau | 3.8% | 32,000 | 2,700 |
| Togo | 3.2% | 110,000 | 9,100 |
| Gambia | 2.4% | 20,000 | 1,300 |
| Ghana | 2.3% | 320,000 | 29,000 |
| Burkina Faso | 2.0% | 150,000 | 12,000 |
| Benin | 1.8% | 87,000 | 9,600 |
| Mali | 1.7% | 130,000 | 11,000 |
| Sierra Leone | 1.6% | 48,000 | 4,600 |
| Guinea | 1.5% | 85,000 | 7,100 |
| Niger | 1.1% | 79,000 | 7,600 |
| Senegal | 0.8% | 44,000 | 35,00 |
| Mauritania | 0.7% | 12,000 | <1,000 |
The region has generally high levels of infection of both HIV-1 and HIV-2. The onset of the HIV epidemic in West Africa began in 1985 with reported cases in Cote d'Ivoire, Benin and Mali. Nigeria, Burkina Faso, Ghana, Cameroon, Senegal and Liberia followed in 1986. Sierra Leone, Togo and Niger in 1987; Mauritiana in 1988; The Gambia, Guinea-Bissau, and Guinea in 1989; and finally Cape Verde in 1990.
HIV prevalence in West Africa is lowest in Chad, Niger, Mali, Mauritania and highest in Burkina Faso, Côte d'Ivoire, and Nigeria. Nigeria has the second largest HIV prevalence in Africa after South Africa, although the infection rate (number of patients relative to the entire population) based upon Nigeria's estimated population is much lower, generally believed to be well under 7%, as opposed to South Africa's which is well into the double-digits (nearer 30%).
The main driver of infection in the region is commercial sex. In the Ghanaian capital Accra, for example, 80% of HIV infections in young men had been acquired from women who sell sex. In Niger, the adult national HIV prevalence was 1% in 2003, yet surveys of sex workers in different regions found a HIV infection rate of between 9 and 38%.
Southern Africa
In the mid-1980s, HIV and AIDS were virtually unheard of in Southern Africa - it is now the worst-affected region in the world. There has been no sign of overall national decline in HIV/AIDS in any of the eleven countries: Angola, Namibia, Zambia, Zimbabwe, Botswana, Malawi, Mozambique, South Africa, the two small states of Lesotho and Swaziland and the island of Madagascar. In its December 2005 report, UNAIDS reports that Zimbabwe has experienced a drop in infections; however, most independent observers find the confidence of UNAIDS in the Mugabe government's HIV figures to be misplaced, especially since infections have continued to increase in all other southern African countries (with the exception of a possible small drop in Botswana). Almost 30% of the global number of people living with HIV live in an area where only 2% of the world's population reside.
Nearly every country in the region has a national HIV prevalence level of at least 10%. The only exception to this rule is Angola, with a rate of less than 5%. This is not the result of a successful national response to the threat of AIDS but of the long-running Angolan Civil War (1975-2002).
Most HIV infections found in Southern Africa are HIV-1, the world's most common HIV infection, which predominates everywhere except West Africa, home to HIV-2. The first cases of HIV in the region were reported in Zimbabwe in 1985.
Impacts of the AIDS Epidemic
Africa's HIV/AIDS epidemic has had important effects on society, economics and politics in the continent. (Source: Tony Barnett and Alan Whiteside, "AIDS in the 21st Century: Disease and Globalization," (MacMillan Palgrave 2003)). The economic impact of AIDS is noticed in slower economic growth, a distortion in spending, increased inflows of international assistance, and changing demographic structure of the population. There are also fears that a major long-term drop in adult life-expectancy will change the rationale for economic decision-making, contributing to lower savings and investment rates. However, most of these impacts remain theoretically possible rather than empirically observed. Economists in South Africa have developed the most sophisticated models for the impacts of the epidemic, and Nicoli Nattrass in "The Moral Economy of AIDS in South Africa" estimates that it is possible for the South African government to provide universal access to anti-retroviral therapy without overstretching the national budget. AIDS has intersected with drought, unemployment and other sources of stress to create what Alan Whiteside and Alex de Waal have called "new variant famine," characterized by the inability of poor, AIDS-affected households to cope with the demands of securing sufficient food during a time of food crisis.
The social impact of HIV/AIDS is most evident in the continent's orphans crisis. Approximately 12 million children in sub-Saharan Africa are estimated to be orphaned by AIDS. These children are overwhelmingly cared for by relatives including especially grandmothers, but the capacity of the extended family to cope with this burden is stretched very thin and is, in places, collapsing. UNICEF and other international agencies consider a scaled-up response to Africa's orphan crisis a humanitarian priority. Practitioners and welfare specialists are sensitive to the need not to identify and isolate children orphaned by AIDS from other needy and vulnerable children, in part because of fear of stigmatizing them. Therefore, there is a search for effective social policies and programs that will provide necessary assistance and protection for all orphans and vulnerable children.
The political impact of the epidemic has been little studied. There has been much concern that high levels of HIV among soldiers and political leaders could lead to a "hollowing out" or even collapse of essential state structures, and an escalation of conflict. Laurie Garrett of the Council on Foreign Affairs is most publicly associated with this position. However, it is also clear that the epidemic has coincided with the entrenchment of democracy in much of Africa, and that governments and armies have learned to cope with the effects of the epidemic.
Spawning new epidemics in Africa and Abroad
Because HIV has destroyed the immune systems of at least a quarter of the population in some areas, far more people are not only developing Tuberculosis but spreading it to otherwise healthy neighbours.
![Changes in life expectancy in several African countries. Botswana has been particularly badly hit [1], while public education projects campaigns have had a positive effect in Uganda [2]. (Source: World Bank World Development Indicators, 2004).](../../images/806/80649.png)